Research conducted by the Centers for Disease Control shows that there are more than 100 million adults in the United States living with diabetes or pre-diabetes. Diabetes occurs when a patient is unable to regulate their own blood sugar levels naturally, and instead rely on controlling aspects of their diet and/or taking medications to help. This is important because when blood sugar levels are too low or too high, it can have a seriously negative effect on our health and wellbeing. Many people don’t realize that diabetes can also affect their vision. It’s for this reason that anyone who is diagnosed with diabetes or pre-diabetes is recommended to undergo regular diabetic eye exams to check for diabetic retinopathy.
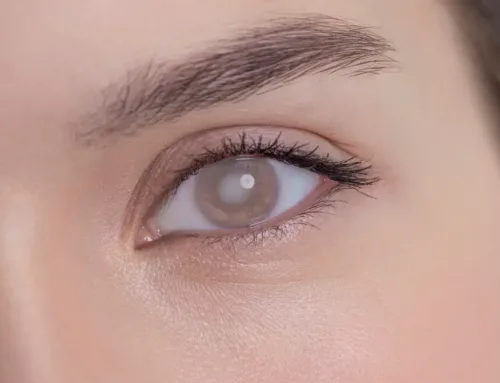
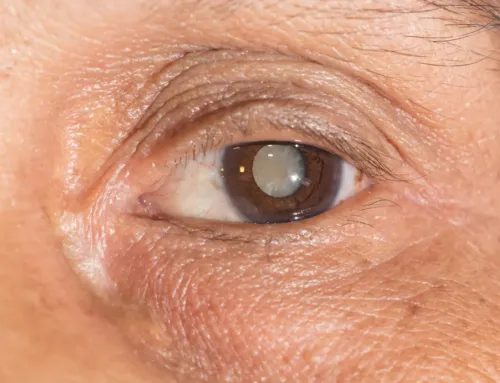
Diabetic retinopathy is the name of the visual complication that can occur as a result of uncontrolled or poorly controlled diabetes. In diabetic retinopathy, persistently high blood sugar levels cause damage to the part of the eye called the retina. The retina is crucial for our vision, converting the light that passes into the eye into signals that are sent to and interpreted by our brains. When high blood sugar levels damage the vessels supplying blood to the retina, it can cause scarring and prevent the retina from working as efficiently as it could. This can impact the quality of your vision. Unfortunately, any vision loss as a result of diabetic retinopathy can’t be restored.
What Happens In A Diabetic Eye Exam?
If you have diabetes or prediabetes, you will probably be invited for an annual diabetic eye exam. This may take place alongside a normal comprehensive eye exam, or as a separate standalone appointment.
Firstly, you will be asked to read letters off of a chart to determine your visual acuity. This will tell your ophthalmologist whether you have a refractive eye error that means that you would benefit from wearing glasses or contact lenses. Your ophthalmologist will require your eyes to be dilated for part of your diabetic eye exam. This is because part of the exam involves looking inside and at the back of the eye. Dilation is very straightforward and involves eyedrops being placed into the eyes. These may sting momentarily, and you’ll find your eyes are more sensitive to light while they are in effect. They will also cause your vision to become blurred. Once your pupils are dilated, a special camera will be used to take images of the inside of your eyes. You’ll be asked into the lens and will see a bright flash as the image is taken. Your ophthalmologist will then use the images to assess the condition of the blood vessels serving the retina to check for any signs of diabetic retinopathy.
In some instances, patients are referred for a special test known as fluorescein angiography. This is where a special fluorescent dye is injected into one of your veins. This dye will travel to the blood vessels serving the retina can reveal changes in the structure and function of the retinal blood vessels.
Can Diabetic Retinopathy Be Treated?
The purpose of regular screening is to try and detect irregular changes to the blood vessels of the retina that occur as a result of diabetic retinopathy before it can affect your vision. In most cases, diabetic retinopathy only requires treatment if it reaches an advanced stage, where your ophthalmologist feels that there is considerable risk to your vision. If you are diagnosed with diabetic retinopathy, you’ll be given advice on getting your diabetes under control, which will help to prevent further damage to your eyes and vision.
If treatment is required, your ophthalmologist will talk to you about the options available, which include laser treatment or injections to prevent the growth of abnormal blood vessels, or surgery to remove scar tissue and blood that may have accumulated in the back of the eye.
If you have diabetes and would like more information about diabetic retinopathy, or if you’d like to schedule a diabetic eye exam in Port St Lucie, FL or Stuart, FL, please get in touch with our dedicated eye care team today.